SPOTLIGHT
New Analysis of Sickle Cell Disease Prevalence Among Medicaid Enrollees Fills Gap in Public Data
Authors:
Client:
PhRMA
November 2023
Updated December 11, 2023
NORC’s Health Care Strategy team analyzed Medicaid claims data (T-MSIS) to identify Medicaid enrollees with sickle cell disease. We found that a majority are Black, and 49 percent have a severe form of the disease and a genotype eligible for recent clinical trials.
Earlier this year, in response to the President’s Executive Order on lowering prescription drug prices, the Center for Medicare and Medicaid Innovation (CMMI) announced three new models to address the affordability and accessibility of prescription drugs. They included the Cell and Gene Therapy Access Model, which aims to increase access to high-cost cell and gene therapies by pooling state Medicaid agencies’ bargaining power, tying the cost of the therapy to its efficacy through outcomes-based agreements, and shifting the administrative burden of the outcomes-based agreements from the individual state Medicaid agencies to the Center for Medicare & Medicaid Services (CMS). While CMMI has not released any details of the model yet, they have indicated that they may test the model on a single indication, such as sickle cell disease.
To better understand this model’s potential impact on access to sickle cell disease treatments, we examined the patient population that may be affected. We did this by analyzing the most recent available year of T-MSIS data (2021) to identify Medicaid enrollees with a sickle cell disease diagnosis. Our analysis fills an existing gap in the literature, as the most recent publicly available data are from a CMS analysis of 2017 T-MSIS data. The 2017 CMS analysis identified 41,995 Medicaid enrollees with sickle cell disease; our analysis identified 52,524 Medicaid enrollees who had sickle cell disease in 2021. The increase in Medicaid enrollees with sickle cell disease is likely due to the increase in Medicaid enrollment between 2017 and 2021. Medicaid enrollment has increased in recent years, in part due to the impact of both Medicaid expansion, which gave states the option to expand Medicaid eligibility to up to 138 percent of the federal poverty level, and the temporary continuous enrollment provision of the Families First Coronavirus Response Act, which incentivized Medicaid programs with the increased federal funding to maintain coverage for enrollees until the conclusion of the COVID-19 public health emergency (PHE).
Individuals with a severe form of sickle cell disease may suffer frequent painful complications called vaso-occlusive crises. We found 49 percent of Medicaid SCD enrollees had a severe form of the disease, based on claims for four or more vaso-occlusive events in a 24-month period—and an SCD genotype that corresponded to eligibility for recent clinical trials.
NORC’s analysis identified 52,524 Medicaid enrollees with sickle cell disease in 2021. These enrollees are disproportionately Black, most likely to be between the ages of 21 and 45, and clustered in Southern states.
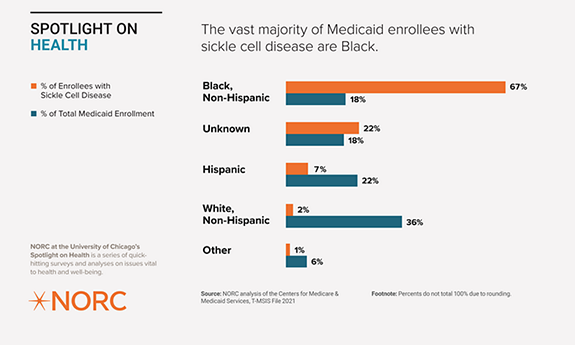
Sickle cell disease disproportionately impacts Black Medicaid enrollees. More than two-thirds (67.4 percent) of Medicaid enrollees with sickle cell disease are Black, despite making up less than 20 percent of total Medicaid enrollment. Excluding the “unknown” race/ethnicity data, Black enrollees make up 87 percent of Medicaid enrollees with sickle cell disease.
Consistent with the existing literature, we found that most Medicaid enrollees with sickle cell disease are Black. Furthermore, by excluding enrollees with an unknown race/ethnicity, the proportion of Black enrollees with the disease rises to 87 percent. Extending access to new cell and gene therapies provides CMMI with the opportunity to address systemic drivers of racial inequities by focusing on diseases that affect Black and other historically minoritized and marginalized populations.
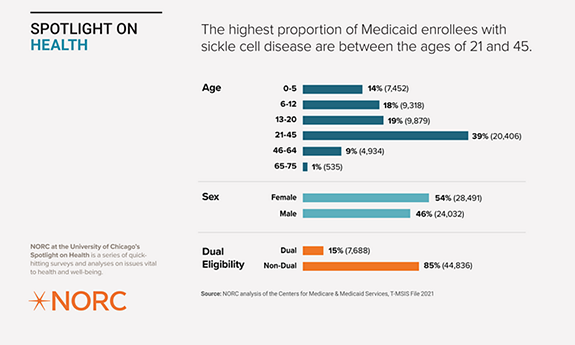
The highest proportion of Medicaid enrollees with sickle cell disease are between the ages of 21 and 45. A slight majority are female, and most are not dually eligible for Medicare and Medicaid.
We found that among the Medicaid enrollees with sickle cell disease, more than a third (39 percent) are between the ages of 21 and 45, whereas only 10 percent are 46 years old or older, which likely reflects the high mortality rate in this population. The majority (85 percent) of the Medicaid population with sickle cell disease is not dually eligible for Medicare and Medicaid, probably because the overwhelming majority of the population is under 65 years old.
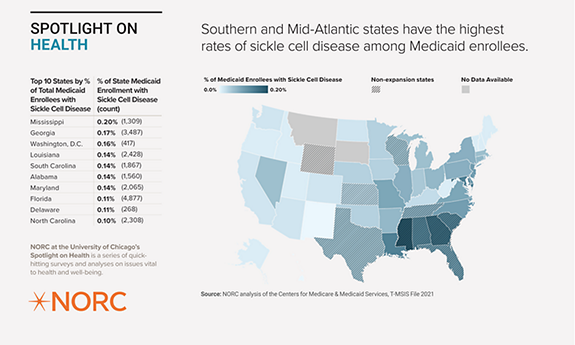
Overall, enrollees with sickle cell disease make up less than one percent (0.07 percent) of all Medicaid enrollees. We found that roughly 49 percent of enrollees with sickle cell disease had both a clinical trial-eligible genotype and a severe form of the disease, characterized by four or more pain crisis events between 2020 and 2021. Sickle cell disease is most prevalent (as a percentage of the total Medicaid population) in Mississippi, Georgia, and Washington, D.C.
We found that the Medicaid patient population with sickle cell disease is not distributed evenly across the country. Southern and Mid-Atlantic states have the highest rates of the disease among their Medicaid enrollees. We also examined the states with the highest counts of enrollees with sickle cell disease, which included New York (5,033), Florida (4,877), Georgia (3,487), Texas (3,211), and California (2,684). Notably, three states had fewer than 11 enrollees with sickle cell disease—Montana, South Dakota, and Wyoming.
Among the top 10 states with the highest sickle cell disease prevalence among their Medicaid enrollees, half did not expand their Medicaid programs following the Affordable Care Act. Medicaid populations in these states tend to be smaller and sicker than expansion state populations, meaning that enrollees with sickle cell disease—who already disproportionately rely on Medicaid—represent a larger proportion of the total.
Methodology
NORC analyzed 2021 T-MSIS data to identify Medicaid enrollees with sickle cell disease. NORC identified enrollees with 12 months of continuous enrollment in Medicaid and at least two sickle cell disease-related claims throughout the year. A sickle cell disease claim was defined as having an ICD-10 code for sickle cell disease in any position. Severe sickle cell disease was defined as having four or more sickle cell disease related claims “with crisis” in the past 24-month period.
Sickle cell disease ICD-10 codes included D57.00, D57.01, D57.02, D57.03, D57.09, D57.1, D57.20, D57.211, 57.212, 57.213, D57.218, D57.219, D57.40, D57.411, D57.412, D57.413, D57.418, D57.419, D57.42, 57.431, D57.432, D57.433, D57.438, D57.439, D57.44, D57.451, D57.452, D57.453, D57.458, D57.459, D57.80, D57.811, D57.812, D57.813, D57.818, D57.819.
Data suppression occurred when any cell contained a value less than 11. If one cell was required to be suppressed due to the cell size limitations, any cells that would enable the researcher to calculate the suppressed value were also suppressed.
Limitations: T-MSIS data have gaps, particularly for certain demographic data, such as race and ethnicity, as they are not required to report race and ethnicity data of enrollees annually or at all. This analysis reflects what data were available in the 2021 T-MSIS file.
This analysis was conducted as part of a larger project with the Pharmaceutical Research and Manufacturers of America (PhRMA). PhRMA commissioned the Health Care Strategy team at NORC to analyze the impacts of the recently announced Cell and Gene Therapy Access Model, a new Center for Medicare and Medicaid Innovation (CMMI) model focused on increasing access to cell and gene therapies to Medicaid enrollees.
UPDATE: On December 11, 2023, this release was revised to correct the percentage of enrollees with a severe form of the disease from 44 percent to 49 percent.







